IT’S ALL CONNECTED! – An ENT Rotation

Corruption: A Moral Cancer
December 29, 2022
Windows to the Soul? – An EYE Rotation
December 29, 2022
IT’S ALL CONNECTED! – An ENT Rotation
After going through a hectic Surgery rotation, ENT felt like a breath of fresh perspective. Being limited to only three structures in the body: ear, nose and throat, opened a new view into what pathologies one can pick out from just three structures in patients, which can be seen with the naked eye or simple instruments. Frankly, having had bouts of runny nose and sore throat with every slight change in weather, I thought it would be dull and gross meeting my archenemies face to face. Fortunately, in the very first week, I made peace with my enemies. Additionally, it was fun to know how connected the ear, nose and throat were; how a nasal polyp would block the Eustachian tube and cause hearing loss, how an inflamed tonsil in the oral cavity causes earache, how a blocked nose causes a sore throat, etc.
There are four essential examinations we do on every patient: ear, nose, oral cavity and neck, and just by performing these, we’re able to pick out signs such as polyps, turbinate hypertrophies, crusting, deviated nasal septums, septal spurs, enlarged tonsils, post-nasal drip, oral ulcers, perforated tympanic membranes, laryngoceles, thyroglossal cysts to name a few. It took a while to figure out whether what I saw was normal or the findings were hiding under my nose (pun intended), but the faculty there would examine the patient again in front of us, and I pat myself on the back when our findings were the same. We’d further discuss the patient’s case on the spot about what investigations would be required and the treatment plan.

Personally, what I especially enjoyed was learning about the ear and its pathologies. In 2nd year, Special Senses was my favourite module, and I enjoyed learning the anatomy and physiology of the eyes and ears. Hence, knowing about disorders affecting hearing and balance, such as acute/chronic suppurative otitis media, labyrinthitis, Meniere’s disease and benign paroxysmal positional vertigo (BPPV), was very interesting to me. Knowing how a tiny cholesteatoma could wreak havoc in the inner ear and brain made me extra cautious in looking for it during an otoscopy examination. I also looked forward to seeing a patient with BPPV to see what the Dix-Hallpike manoeuvre looked like and how it would instantly improve vertigo.

The calls were quite fun. We were meant to go once a week, on Monday, Tuesday or Friday, where we’d take histories and examine patients before presenting the cases to Dr. Zafar. There were some interesting cases to see in the SIH OPD. There was one adorable boy who was eight years old with a deviated nasal septum and allergic rhinitis. I started with taking the history from his father, but instead, the boy answered my questions so fluently that I thought, “Woah, this kid can speak.” I proceeded to ask him questions. When I asked about his allergic history, he had a skin prick test is done, which tests for multiple allergens, whose result was that he was allergic to dust, peanuts, almonds, and even chicken! I couldn’t help saying, chicken?! Then how would you enjoy a KFC?” He replied, “I still eat chicken anyways.” I couldn’t figure out whether to high-five him or tell him to chill.
Nonetheless, the kid was adorable. I remember we were taking a history of another patient who only complained of neck pain, with no ENT-related symptoms whatsoever, but we worried that Dr. Zafar would ask us for the differential diagnoses while we were blank. Thankfully, he just had a muscle sprain, so we sighed in relief.
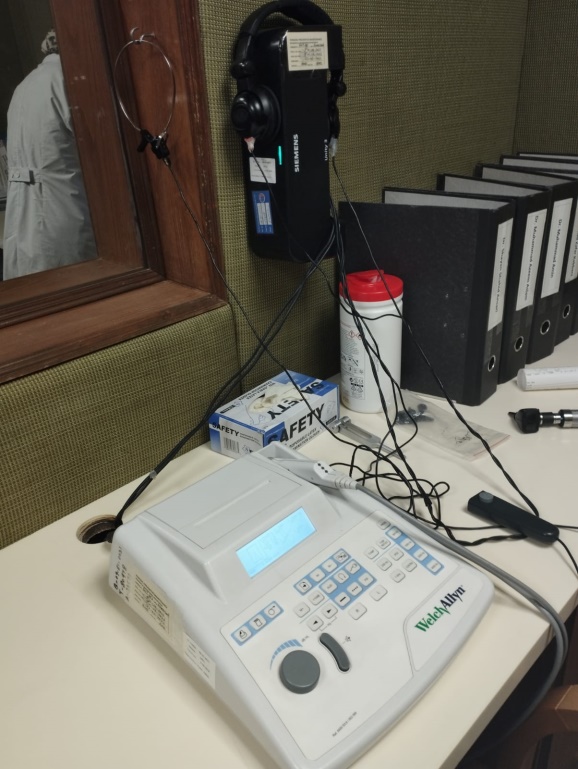
We saw a patient’s Pure Tone Audiometry done to check his hearing. The patient was taken to the audiology room where the walls were covered in foam to dampen vibrations of sound, and the patient was supposed to wear a headphone where sound waves of specific frequencies were transmitted, and if he could hear the sound, he would press a button, and it would be plotted on the PTA chart on the computer. While we observed him and the chart in the adjoining room, he’d be in a separate room. It was pretty cool seeing how the hearing was practically assessed.
Lastly, we would go to the OR every Tuesday and Thursday and observe adenotonsillectomy, where the adenoids and tonsils are removed; septoplasty, where the deviated nasal septum is repaired, functional endoscopic sinus surgery (FESS), where the sinuses are opened, and polyps are removed, and myringotomy, where a small knife is used to make a hole in the tympanic membrane of the ear and a grommet, is inserted to allow for accumulated pus in the middle ear to be drained out. We were given the option to scrub in during adenotonsillectomy so we could better visualise the tonsils and hold the suction tube to suck out blood and smoke produced from electrical cauterisation. Adenoidectomy was quite disturbing as they put a sharp instrument through the oral cavity, and with one swipe, they scraped off the adenoids, which came out as a small, fleshy mass. Nevertheless, the environment in the OR was very relaxing, with the entire faculty teaching and accommodating us, the best of whom being Dr. Zafar, who would occasionally crack jokes and ensure a light, fun and relaxed environment in the OR for everyone.
I sign off with a picture of me holding this cute, squishy buddy Dr. Zafar handed to us in the OR as soon as we came in:

So that was my ENT rotation. How was yours? Let me know in the comments below
_ _ _ _ _ _ _ _ _
Nahin Sani
MBBS Class of 2023
