Windows to the Soul? – An EYE Rotation

IT’S ALL CONNECTED! – An ENT Rotation
December 29, 2022
Certificate of Appreciation by CDA – Annual Tree Plantation Activity
February 17, 2023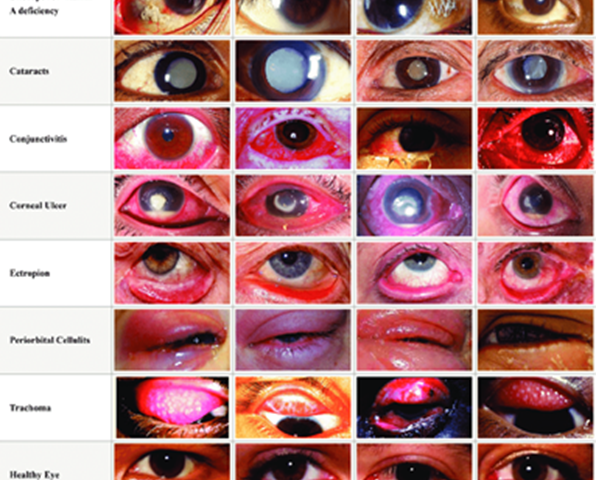
Wearing glasses since I was five years old and hearing how every second person I came across had laser eye surgery, eyes have had particular importance in my life. I remember when I was little, I was told that if my eye’s refractive errors reached -8, I would go blind, so with age, as my number became more negative, I was terrified of the prospect of never being able to see again. In addition, I had another fear that if anything penetrated my eye even the slightest such as a bobby pin or anti-lice lotion, I’d immediately go blind forever. Thankfully, as my brain cells matured and through learning from this rotation, I realized things weren’t as severe as I believed them to be.
Many myths we were told about our eyesight were clarified during this rotation. For example, our vision doesn’t grow weaker because of excessive screen time; its incidence increases but doesn’t cause worsening eyesight. Furthermore, a positive value of refractive error (hypermetropia) doesn’t always mean that near vision is weak. Hypermetropia and myopia are terminologies both used for far vision; the difference is only in whether the image is focused in front of (myopia) or behind (hypermetropia) the retina when looking at a distant object. Presbyopia (age-related decrease in vision) is a decline in near vision. Additionally, our vision doesn’t weaken by wearing someone else’s glasses.
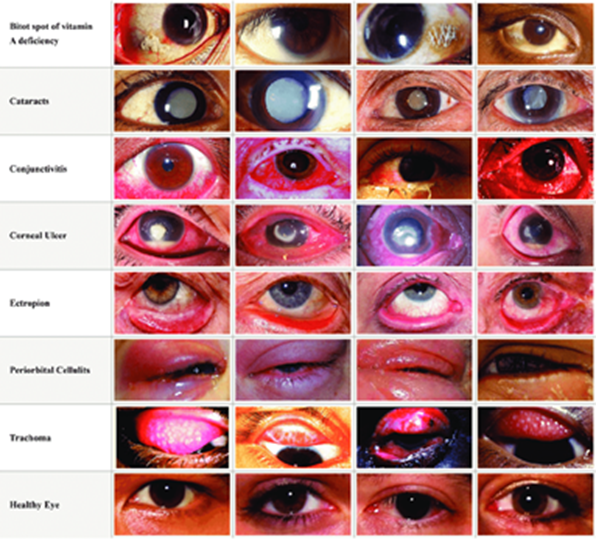
In this rotation, like ENT, it was exciting to pick out findings through the naked eye or ophthalmoscope and confirm them on the spot by the faculty. You can assess patients’ visual acuity as easily as your own by making them read the Snellen chart. You can pick out multiple findings in the eye, even in the comfort of your home through your torch, such as cataracts, glaucoma, corneal opacity, artificial lens, heterochromia (difference in colour) of the iris, hypopyon (pus in the anterior chamber), hyphema (blood in the anterior chamber), pterygium (triangular shaped growth from the conjunctiva encroaching the iris) to name a few. The torch can also check for pupillary reflexes and relative afferent pupillary defect (RAPD). Once I picked out what I thought was RAPD but was doubtful about it, I decided to tell our preceptor that I felt it was RAPD. When she confirmed my finding, I loudly whispered, “Yes!” and realized that my first instinct is often true, so I shouldn’t doubt it.
There was one patient I remember who complained of decreased vision in his left eye for ten years after having been hit in the eye by a marble by his family member. RAPD was positive; he was aphakia (absence of lens) as his iris was tremulous, and fundoscopy showed optic disc cupping. Before presenting the case, the patient was repetitively asking whether his vision would improve. A slit lamp examination revealed that he had a macular scar, and the doctor said that his vision would not improve. I didn’t want to imagine how that patient felt after knowing the outcome of being hit by an ordinary and often safe-playing object like a marble.
Ophthalmoscopy was a challenge to learn how to use and see the fundus of the eye correctly because whenever I’d move close to the patient’s eye, the image would become blurred, and I’d only see the reflection of the light coming from the ophthalmoscope. On a few occasions, by the end of the rotation, I could spot some retinal vessels and the optic disc but that was the best I could do.

Other examinations include confrontational visual field, digital tonometry, regurgitation test, ptosis and squint examination. I think many people can agree with me that squint was a challenging concept to understand. Nevertheless, in the end, the faculty members would simply check every patient with a slit lamp and complete their examination in a few minutes. I hoped a monitor would display what they would see through the slit lamp because more than one person couldn’t look through the lens simultaneously, but the faculty discussed the case and the findings they found in detail.
We were told to alternate between working in the Falahi and SIH OPDs because we could practice our history-taking skills and examinations in Falahi. In contrast, we could see a greater variety of cases in SIH OPD, such as retinal detachment, glaucoma, keratoplasty (corneal transplant), keratoconus (thin and cone-shaped cornea), trauma to the eye causing permanent loss of vision, vitreous haemorrhage and Behcet’s disease. One time, a consultant had to remove a suture from a patient’s eye where keratoplasty was done, which was very creepy to watch and made me flinch. Thankfully in one procedure room, there was a screen through which I could see what the consultant could see through the slit lamp.

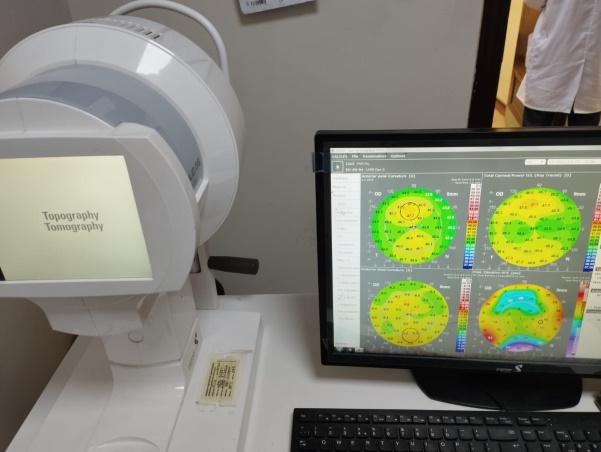
In the SIH OPD, there were a lot of high-tech instruments used for investigating eyes such as Optical Coherence Tomography (OCT) to check the macula and optic disc for macular degeneration and glaucoma, automated biometry to check visual fields, B-scan which is an ultrasound of the eye, and corneal topography which assesses the curvature of the eye as shown in the picture below, similar to assessing the topography of the land. One of the operators was especially kind in showing me the OCTs of multiple patients with glaucoma or age-related macular degeneration.
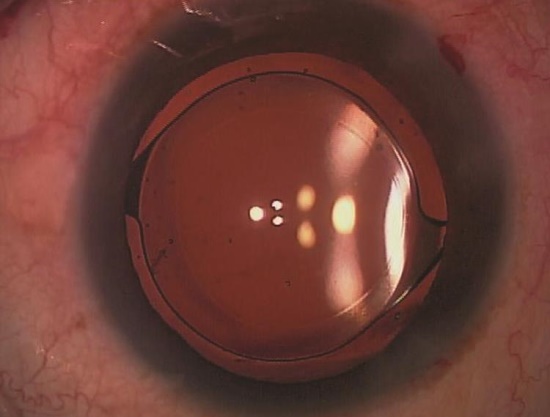
We also observed a cataract surgery in the OR located in the Falahi department. It was phacoemulsification, precisely where a probe is inserted into the lens capsule that sends ultrasound waves that break down the sclerotic lens into smaller fragments. Once that’s done, the same probe is used for suction to remove the fragments from the lens. Afterwards, a foldable artificial intra-ocular with a refractive index specific to the patient’s need is placed. Once released inside the lens capsule, the lens unfolds on its own. One thing that bothered me was that the patient was under local instead of general anaesthesia, so although the patient was not in pain, wouldn’t it be scary or uncomfortable for the patient to see multiple instruments move in front of them and poke into her eye? I asked the consultant this, and she said that the light source used during the surgery was so bright that the patient could not see what was going on with her eye. Her answer was confirmed in a few seconds by the sound of snoring.
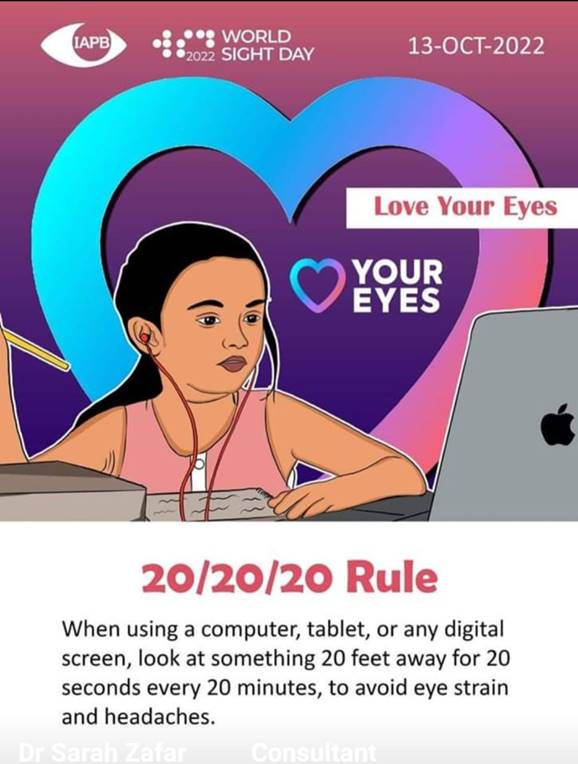
Overall, it was a fun, relaxed and informative rotation. I shall end this article with a picture sent by our Clerkship director:
_ _ _ _ _ _ _ _ _ _
That was my Eye rotation. How was yours? Let me know in the comments below
Nahin Sani MBBS Class of 2023
